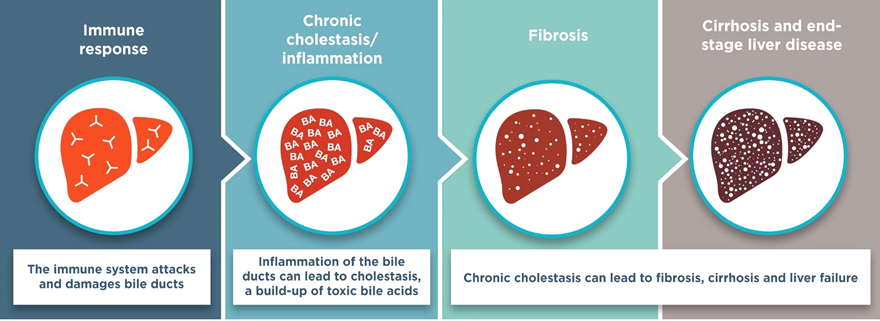
Biliary fibrosis is a liver disease caused by inflammation that ultimately leads to scarring of the liver. This is a common symptom of biliary atresia, a rare congenital childhood disorder that causes bile to be trapped in the liver; this causes fibrosis. Previous research showed that a population of hepatic progenitor cells expressing the stem cell marker Prom-1 expanded in the diseased liver of adult biliary fibrosis patients. In the current study, researchers from the Children’s Hospital of Los Angeles expanded this association to show that these Prom-1-expressing liver cells are also associated with biliary fibrosis in biliary atresia patients, and identify the signaling pathway responsible for this effect.
The Bioss anti-LacZ antibody was used to validate the Prom-1 knockout mouse strain used in all of the experiments in this study. In order to knockout Prom-1, the gene for LacZ was inserted into the prominin-1 gene locus, which encodes Prom-1. Therefore, the presence of LacZ would indicate an absence of functional Prom-1. Immunostaining for LacZ in the Prom-1 knockout mice showed the same pattern of staining as did Prom-1 in wild-type mice, indicating that the knockout mice have the expected phenotype.
Prom-1 knockout mice as well as wild-type mice were then infected with RRV - rhesus rotavirus - which induces biliary atresia. First, the authors investigated whether symptoms of biliary atresia were resolved in the absence of Prom-1. In both wild-type and knockout mice, bile ducts located outside the liver were equally as damaged by RRV infection. However, in the liver, Prom-1 knockout mice did not exhibit signs of liver damage including inflammation, an increased number of bile ducts, or fibrosis.
Surprisingly, this difference could not be attributed to a difference in the amount of pro-inflammatory cytokines present in the liver. Instead, the changes were due to differential activation of the TGF-beta pathway, which is known to be involved in the progression of many liver diseases. Integrin-beta 6, which can activate TGF-beta, was nearly absent in the livers of Prom-1 knockout mice with biliary atresia. In wild-type mice with biliary atresia, Prom-1 was highly expressed around the bile ducts. These results indicate that Prom-1 can control the expression of integrin-beta 6. Integrin-beta 6 can then activate the TGF-beta pathway, which drives biliary fibrosis.
Indeed, when the researchers looked for a correlation between Prom-1 and markers of biliary atresia symptoms, they found that markers of bile duct formation and fibrosis were correlated with Prom-1 expression. In patients that were successfully treated for their biliary atresia, expression of several of these markers was significantly decreased compared to patients who failed treatment.
Finally, the authors wanted to determine whether the pathway driven by Prom-1 played a role in other childhood liver diseases besides biliary atresia. Patients with indeterminate cholestasis had normal levels of Prom-1 and integrin-beta 6 and did not have signs of an increased number of bile ducts or fibrosis. Therefore, Prom-1-driven fibrosis is specifically a symptom of biliary atresia, and not other liver diseases. Because Prom-1 has now been identified as a specific marker of biliary fibrosis in biliary atresia patients, researchers may look into Prom-1 as a potential target of treatment for this disease.